When prescribed antibiotics, healthcare professionals advise patients to take the full course of the medication to ensure that the infection is properly treated. Non-adherence to this standard has been thought to have contributed to the rise of antibiotic-resistant superbugs.
Why do we have to take long courses of antibiotics?
The fact is, the longer you take an antibiotic for, the greater the chance that antibiotic-resistant bacteria will emerge in your body and in the environment around you. There are some chronic infections, such as tuberculosis, where you do indeed have to take long courses of antibiotics, not to prevent resistance, but rather to cure the infection.
Why do we prescribe antibiotics?
We've long prescribed antibiotics out of fear and habit, not science. Indeed, as far back as 1945, Alexander Fleming, the man who discovered penicillin in 1928, warned the public that people were taking penicillin to treat diseases not caused by bacteria, and that this unnecessary use of penicillin was going to breed out antibiotic resistance.
Should you complete your antibiotic prescription?
The World Health Organization still advises patients to “always complete the full prescription, even if you feel better," but there is no scientific evidence that supports the claim. The CDC and Public Health England in recent years have replaced “complete the course” with messages advocating taking antibiotics “exactly as prescribed.”
Why do antibiotic treatment guidelines vary by patient level?
Antibiotic treatment may vary on a patient level due to previous exposure to certain antibiotics and individual response to therapy; however, current guidelines do not account for these factors, according to the study.
Does stopping antibiotics increase resistance?
Can antibiotics cause recurrent infections?
About this website
Why Not To Beg Your Doctor For An Antibiotic - Majic 102.1
“There are approximately 13 or 14 million visits every year to doctors and emergency rooms for sore throat and more than 50% get antibiotics when it’s pretty clear that strep throat is quite uncommon,” says Mary Caserta, MD, an associate professor of pediatrics at the University of Rochester Medical Center, in New York.
Experts: End ‘complete the course’ for antibiotics - WebMD
July 27, 2017 -- The message given by doctors to "complete the course" when taking antibiotics should be dropped, experts say.. They argue that it is not backed by evidence and should be replaced.
Why finishing your Antibiotics is still important - NHS - Healthy ...
Please dont stop using Antibiotics because of todays news . Today the Telegraph and many other newspapers published a top of the frontpage article in which the headline suggested patients shouldn’t complete their courses of Antibiotics, but stop Antibiotics when they feel better. I believe this is irresponsible journalism considered the public health implications such a message carries.
What danger will result from not completing a course of prescribed ...
I think the danger of creating antibiotic-resistant bacteria is very real. Bacterial infections, before antibiotics, quite often proved to be fatal and by discontinuing a course of prescribed ...
How long should antibiotics be given?
Here’s the bottom line 1 Antibiotics are a limited resource, and they should be used wisely and selectively. 2 Antibiotics may also have serious side effects, such as the major intestinal ailment Clostridium difficile colitis. 3 There is no evidence that longer courses prevent the development of antibiotic resistance. In fact, just the opposite may be true. 4 Instructions about length of antibiotic therapy are sometimes arbitrary, and some patients may recover faster and need fewer days of antibiotics than others. 5 You should still follow your doctor’s instructions about the length of antibiotic therapy. 6 If you are feeling better and think that you may not need the entire course, be sure to ask your doctor first. 7 Antibiotic administration is not necessary for all infections. In particular, most upper respiratory infections are viral, and do not respond to antibiotics.
How long should I take antibiotics after symptoms disappear?
As a pharmacist with 40 years of experience, I tell patients who ask to take the antibiotic for at least 72 hours after symptoms disappear completely.
How long does it take for a bloodstream infection to cure?
Today, we know that patients with bloodstream infections may require several weeks of antibiotics for cure, and those with active tuberculosis need many months of multiple antibiotics. But these patients are not representative of most people who receive antibiotics today.
What is the blood test for antibiotics?
Doctors are studying new clinical tools to help limit unnecessary antibiotic use. One of these is a blood test called procalcitonin. Levels of procalcitonin rise in patients with serious bacterial infections. In patients with viral infections, which do not respond to antibiotics, procalcitonin levels are suppressed.
Can antibiotics cause colitis?
Antibiotics are a limited resource, and they should be used wisely and selectively. Antibiotics may also have serious side effects, such as the major intestinal ailment Clostridium difficile colitis . There is no evidence that longer courses prevent the development of antibiotic resistance. In fact, just the opposite may be true.
Is antibiotic resistance a threat?
Antibiotic resistance is an emerging threat to public health. If the arsenal of effective antibiotics dwindles, treating infection becomes more difficult. Conventional wisdom has long held that stopping a course of antibiotics early may be a major cause of antibiotic resistance. But is this really supported by the evidence?
Can antibiotics cause bacteria to colonize?
In a few of the studies, researchers looked at the risk of having antibiotic-resistant bacteria on the body after antibiotic therapy. Compared to those who received longer courses of antibiotics, patients who received fewer antibiotics had either the same or a slightly lower risk of being colonized by antibiotic-resistant bacteria.
Why do you need to stop antibiotics?
So why is it that your doctor recommends finishing your course of antibiotics? It's because taking them regularly until the prescription is complete helps ensure that all of the illness-causing bacteria are killed or prevented from multiplying. Even if your symptoms go away, the bacteria may still be present in your body. If you stop treatment before the antibiotic cycle is over, the remaining bacteria can continue to multiply. If these bacteria become resistant to the antibiotics, they can potentially do even more harm. It may take longer for you to recover from your illness, and your physician may have to prescribe more medication.
What are the diseases that can be treated with antibiotics?
Antibiotics are medicines that treat bacterial infections by either killing the bacteria or making it more difficult for them to grow and multiply. Illnesses that can be treated by antibiotics include respiratory tract infections such as whooping cough and pneumonia, as well as skin infections. While antibiotics don't treat most colds, which come from viral infections, they do treat strep throat, as it's caused by streptococcus bacteria.
What is the difference between amoxicillin and penicillin?
Broad-spectrum antibiotics such as amoxicillin affect a wide range of bacteria, while narrow-spectrum antibiotics like penicillin only affect a few different types of bacteria.
What to do if you miss an antibiotic?
Talk to Your Doctor. If you're concerned about your ability to finish an antibiotic course, be sure to ask your doctor what will happen if you miss a dose. You may be able to take the forgotten pill as soon as you remember, or you may have to wait until your next dose.
Can you shorten your antibiotics?
If you're anxious to stop taking your prescription early, ask your doctor if it's OK -- there may be certain instances when it won't hurt to shorten an antibiotic course. One study found that a two- to four-day course of antibiotics was just as effective as a conventional seven- to 14-day regimen in eradicating a urinary tract infection in children.
Can you take antibiotics if you have a bacterial infection?
If you've ever had a bacterial infection, you've probably been prescribed antibiotics to treat it . You also likely remember your doctor telling you that it's important to take all your pills, even after your symptoms have gone away.
Can antibiotics cause bacteria to multiply?
If you stop treatment before the antibiotic cycle is over, the remaining bacteria can continue to multiply. If these bacteria become resistant to the antibiotics, they can potentially do even more harm.
Why did antibiotics evolve?
The authors wrote that the bacteria evolved because of target selected resistance.
What are the pathogens that drive drug resistant infections?
Bacteria, such as Escherichia coli and ESKAPE organisms, are opportunistic pathogens that take hold in vulnerable patients. These bacteria are currently driving drug-resistant infections.
Can antibiotics cause resistance?
The authors suggest that patients may be at risk of developing antibiotic resistance from longer-term treatment opposed to when it is stopped early, according to the study.
Do antibiotics need to be completed?
In contradiction to traditional guidelines, findings from a new study published by BMJ suggest that completing a course of antibiotics may not be necessary. The authors said that the recommendations should be revised to reflect current scientific findings.
Can you stop antibiotics until full course is completed?
The authors argue that the standard concept of not stopping antibiotics until the full course is completed may not be supported by scientific evidence; however, exposing patients to longer courses of antibiotics may increase the likelihood of developing resistance.
How long should you take antibiotics?
321 that the week would consist of seven days. That's why your doctor gives you seven or 14 days ' worth of antibiotics!
How much antibiotics are unnecessary?
It has been estimated that 30 to 50 percent of antibiotic use in the U.S. is unnecessary. In my opinion, those numbers are rather hilariously low. I would that estimate 75 percent or more of antibiotic use is unnecessary. You see, I, and experts like me, have a more stringent definition of when antibiotic use is appropriate or not, which includes giving too long a course of antibiotics to patients who need them.
What to say when your doctor says antibiotics?
If you are sick and your doctor mentions antibiotics to you, the first thing you should say is, "Hey, doc, do I really need the antibiotic?"
Can you stop antibiotics after taking them?
Third, after you begin taking the antibiotics, if you feel much better before you complete the course, give your doctor a call and ask if you can safely stop therapy. So, the bottom line is, doctors should prescribe as short a course of antibiotics as possible to treat your bacterial infection.
Can you take antibiotics past?
Not only is there absolutely no evidence that taking antibiotics past when you feel better will reduce antibiotic resistance, it doesn't even make sense. The fact is, the longer you take an antibiotic for, the greater the chance that antibiotic-resistant bacteria will emerge in your body and in the environment around you.
Does shorter course antibiotics lower resistance?
Furthermore, the shorter-course regimens led to lower rates of antibiotic resistance.
Is it better to take a shorter course of antibiotics or a longer course?
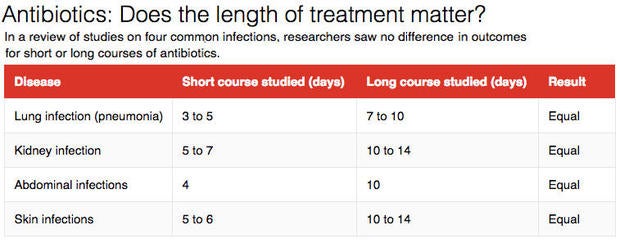
But in the last two decades, we actually have had dozens of clinical trials published demonstrating that shorter courses of antibiotics are just as effective as longer courses (see table).
Why do you need to take antibiotics over the prescribed course?
This requires that you take all your antibiotics over the prescribed course in order to maintain a high enough concentration of the drug to fully penetrate the biofilm. Without going to far into pharmacodynamics, your liver breaks down antibiotic compounds as they circulate through your blood. This means that you must keep taking the antibiotic to keep the concentration in your blood high enough.
Why not take antibiotics for full course?
So what does this mean from a practical standpoint? Not taking your antibiotics for the full course is unlikely to create an antibiotic resistant strain of bacteria. It increases the possibility, but it's unlikely. The largest reason why you are to finish your full course is to prevent the dormant bacteria from replicating and making you sick all over again.
What happens if you stop antibiotics early?
If you'd finished your course, those resistant bacteria would have all been finished off, but by stopping early, you turn yourself into a factory for producing antibiotic resistant bacteria.
What makes some bacteria more sensitive to antibiotics than others?
Others have small mutations that make the antibiotic less effective, and some bacteria produce enzymes that break down antibiotics.
How do biofilms help bacteria?
Since there are so many bacteria in close proximity, it facilitates the transfer of resistance genes throughout the colony via horizontal gene transfer. In addition, one species of bacteria may have the capacity to inactivate an antibiotic, allowing other susceptible species to survive.
How long should you stop taking antibiotics?
So the recommended 5/7/10 days is a number of days which most infections take to fight sufficiently.
Is antibiotic resistance genetic?
This is separate from the traditional sense of "antibiotic resistance", where a genetic mutation causes the antibiotic to stop working by altering a target (or via some other modification). In this case, it's not genetic, but almost 'behavioral'. The bacteria are altruistically ceasing their own replicative capacity temporarily in order to ensure the survival of the colony. Inclusive fitness at its finest.
What percentage of antibiotics are inappropriate?
Total “inappropriate” antibiotic use, which includes incorrect dosing and duration, is nearly 50 percent.
What was the name of the drug that scientists used to treat a man's infection?
Researchers cited an example from 1941 in which scientists treated a man’s infection with penicillin, only for the infection to eventually reemerge and kill him when doctors ran out of medicine.
What is the message of taking until you feel better?
Doctors would have to convey a message to patients that is both safe and effective. A message such as “take until you feel better,” is somewhat ambiguous and could create problems in an outpatient setting. “What people are tolerant of in terms of symptoms can matter,” said Olden.
What is the first phase of the Complete the Course?
The first phase is to establish research to show what is a minimum effective dose for different kinds of antibiotics. The second phase concerns how to best promote that message. Part of the appeal of the “complete the course” message has been its simplicity. Doctors would have to convey a message to patients that is both safe and effective.
Is antibiotic resistance a global health threat?
Antibiotic-resistant bacteria is considered a major global health threat, but at the same time antibiotics are being prescribed more than ever. According to the Centers for Disease Control and Prevention (CDC) Trusted Source. , roughly 1 in 3 antibiotic prescriptions outside of a hospital setting are unnecessary.
Can you take antibiotics as scheduled?
Patients have always been told that the key to a safe and effective course of antibiotics is to take all your pills as scheduled, even if you feel better.
Is the complete the course message unnecessary?
Researchers argue that not only is the “complete the course” message unnecessary, it is actively contributing to the growth of antibiotic-resistant bacteria — not preventing it.
How long does it take to finish an antibiotic?
And for the last 75 years, people with a bacterial infection have been told it is essential to finish all of an antibiotic prescription, usually seven to 10 days, ...
How long is a short term course of antibiotics effective?
In pneumonias that were acquired in the hospital, for example, randomized-controlled trial data indicates that short-term medication courses — for three to five days — is as effective as longer courses and were associated with lower rates of infection recurrence and antibiotic resistance.
How long does it take for a child to feel better after taking antibiotics?
In other words, if a child feels completely better after five or six days out of a 10-day course, it's safe to stop.
Why do we need to wipe out bugs?
The worry has long been that an infection must be wiped out so that any surviving bugs don't become resistant. This deeply embedded message is being put into question by a group of UK experts in a research analysis published Wednesday in the British Medical Journal on Monday. Martin Llewelyn, lead author of the study, and many other experts are saying that “ completing the course ” of antibiotics may be unnecessary.
When is antibiotic resistance put at risk?
Patients are put an unnecessary risk from antibiotic resistance when treatment is given for longer than necessary, not when it is stopped early, British researchers say. Shutterstock
Does antibiotic treatment reduce the risk of resistant infections?
According to the report, an individual’s risk of resistant infection depends on how much of an antibiotic they've taken in the past, so reducing exposure with shorter courses of antibiotic treatment is associated with lowered risk of resistant infection.
Can antibiotics be prescribed for viral infections?
Already doctors have been more cautious about prescribing antibiotics, especially for viral upper respiratory infections. "We only want to be treating for bacterial infections," Azar said, noting you should ask your doctor to perform a culture so you know what bug she's treating.
Why do we have to take antibiotics?
The idea that you have to take all the antibiotics you’re prescribed is based on the assumption that all the bacteria causing the infection have to be killed, so the surviving minority don’t become resistant. In fact, for most otherwise healthy people, significantly reducing, but not necessarily totally eliminating, the bacteria causing the infection allows the body’s natural defences to take over and mop up the remaining few.
Why are antibiotics misused?
Antibiotics have saved countless millions of lives, but have been often misused because of the misguided belief that they are harmless. The most important – but hardly novel – message for doctors is “don’t prescribe antibiotics unnecessarily, especially for colds and flu, ...
How long does the effect of antibiotics last?
The effect lasts for weeks, and the longer the antibiotic course, the greater the risk that antibiotic-resistant bacteria will take their place and cause harm. What’s more, they can spread to other people and add to the pool of antibiotic resistance in the community.
Why is it important to kill all bacteria?
There are some special circumstances when it’s important to kill all the bacteria – when the patient’s normal defences are damaged for any reason, for instance, or when the infection is in a site that’s relatively inaccessible to antibiotics and the white blood cells that kill bacteria. This can be in the middle of an abscess or cavity filled ...
What is the general rule of the shortest course?
The general rule is: the shorter the course, the lower the risk of side effects or resistance. More trials are needed to determine the shortest courses that can be recommended without increasing the risk of relapse. But ultimately, it will still depend on clinical judgement not arbitrary rules, conventions or package inserts.
Is the rate of antibiotic resistance proportional to the amount of antibiotics used?
The right dose. The rate of antibiotic resistance (in a community, a hospital or a whole country) is proportional to the total amount of antibiotics used. The relationship is complex but the dangerous increase in multidrug-resistant bacteria has led some experts to predict the “end of the antibiotic era”. This is the downside of 75 years of ...
Do antibiotics cause allergies?
Antibiotics are generally benign but they all cause allergies and other rare side effects in a small proportion of people. And there’s a universal effect that’s less well known – even a very short course will kill many of the friendly bacteria in the gut.
Does stopping antibiotics increase resistance?
The original article bases its findings on a very limited set of clinical trial data for some specific infections. Their main argument is that in the trials they examined, there was no evidence that stopping treatment early increased a patient’s risk of resistant infection. Conclusive? Hardly. Let’s think about the possible microbiological outcomes when you stop taking your antibiotics early.
Can antibiotics cause recurrent infections?
If the latter is true, the persistent population in your body that is causing your recurrent infection could well be resistant to that first set of antibiotics, meaning those antibiotics may well be useless against your infection.
Popular Posts:
- 1. what to do after andrew ng course
- 2. what is a humanties course uf
- 3. of course you don't need all those attachments but why woulnd you southpark bike
- 4. what is the advanced special operations course
- 5. how many weeks before a course representative can make revisions qm
- 6. how to remove a course still on the canvas dashboard
- 7. how much is take one college course class
- 8. what is the average revenue of a us golf course
- 9. what are the physical stàndards for certified police officer training course new york state
- 10. how do i grant access to my udemy course