According to the Merck Manual, this discomfort lasts for about one to two seconds at a time. Once pulp necrosis develops, you can’t feel cold at all. However, you might feel heightened pressure in the affected tooth from eating or grinding your teeth. This pressure also lasts for several minutes at a time, compared to just a couple of seconds.
Full Answer
What does it mean when pulp necrosis dies?
Feb 01, 2018 · Eventually, the pulp can die. Another cause of pulp necrosis is chronic pulpitis. This involves long-term inflammation (swelling) of pulp from long-term decay, trauma, and multiple large restorations.
What is the difference between irreversible pulpitis and necrosis?
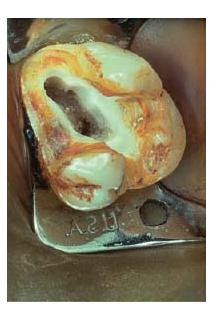
Mar 22, 2022 · Dental pulp necrosis is the final stage of an infection inside the tooth called pulpitis. Pulpitis most often starts with tooth decay or a cracked or broken tooth. Too much drilling into a tooth or other invasive procedures can also be a cause. Any of these conditions can allow bacteria to get into the pulp chamber, allowing an infection to grow.
What are sequelae of a necrotic pulp?
Pulp necrosis is a clinical diagnostic category indicating the death of the pulp and nerves of the pulp chamber and root canal of a tooth which may be due to bacterial sequelae, trauma and chemical or mechanical irritation. It is often the end result of many cases of dental trauma, caries and irreversible pulpitis. In the initial stage of the infection, the pulp chamber is partially …
What is the pathophysiology of necrosis?
In contrast to teeth with vital pulp tissue, teeth exhibiting pulp necrosis frequently exhibit bacterial contamination and may require a different approach to treatment. 318 Sjögren and colleagues 290 raised questions regarding the long-term prognosis of teeth exhibiting necrotic pulp tissue and apical periodontitis treated in a single visit.
How long does pulp necrosis take?
As a side note, it usually takes approximately three months for radiographic changes of pulpal necrosis to become evident with a periapical lucency, for instance, and please remember these lucencies aren't always clear or evident.Feb 19, 2020
How do I know if my pulp is necrotic?
The diagnosis of pulp necrosis can be based on the following observations: negative vitality, a periapical radiolucency, a grey tooth discoloration and even peri-apical lesions. This altered translucency in the tooth is due to disruption and cutting off of the apical neurovascular blood supply.
What happens after pulp necrosis?
What Are the Complications of Pulp Necrosis? Untreated pulp necrosis can lead to more severe problems, including: Sinus infections. A dental abscess, which is a buildup of pus around the tooth and gum.Apr 12, 2021
How long does pulp inflammation last?
Symptoms and Signs of Pulpitis When the stimulus is removed, the pain ceases within 1 to 2 seconds. In irreversible pulpitis, pain occurs spontaneously or lingers minutes after the stimulus (usually heat, less frequently cold) is removed.
How do you know if pulpitis is reversible?
If your pain occurs with temperature extremes but goes away quickly, you may have a reversible condition. But if the pain is intense, lingers after temperature changes, occurs spontaneously, or is referred to other teeth, making it hard to determine the exact location, you may have irreversible pulpitis.
Will antibiotics help gangrenous pulp?
A dentist will not recommend systemic antibiotics as a treatment for irreversible pulpitis. This is because antibiotics will not alleviate the pain and heal the nerve inside the tooth.Mar 3, 2020
How do you treat necrotic pulp?
Treatment optionsFillings. Your dentist may fill existing cavities to prevent further decay of the tooth. ... Root canal. In this procedure, your dentist removes dead tissues throughout the pulp chamber and root of your tooth to eliminate infection. ... Pulp removal. ... Tooth replacement.Feb 1, 2018
Can tooth pulp heal itself?
Unfortunately, the infected pulp of the tooth will not heal on its own and requires a root canal to properly be treated. Sometimes, patients may think a tooth infection has healed itself once they no longer feel pain in their tooth, but this just signals that the nerves inside of the tooth have died.
What is a definite indication of pulp necrosis?
If pulp necrosis and infection of the coronal fragment occurs, there will be radiographic signs of bone loss at the level of the fracture. Symptoms, such as pain, excessive mobility, gingival swelling or a draining sinus, may also indicate that the coronal pulp has necrosed and become infected.
How long does it take for an inflamed tooth nerve to heal?
Pain should subside within a week or so and sensitivity should stop after two to four weeks. If it continues for longer, contact your dentist.Oct 19, 2020
How do you calm pulpitis?
Over-the-Counter Pain Relievers for Pulpitis When taken in normal doses, NSAIDs (nonsteroidal anti-inflammatory drugs) like ibuprofen or non-opioid analgesics like acetaminophen can help manage the pain of pulpitis. Higher doses may be needed to reduce inflammation. These drugs are a good option for most people.Jul 30, 2019
Can pulpitis spread?
Irreversible pulpitis may lead to a type of infection called periapical abscess. This infection develops at the root of the tooth, where it causes a pocket of pus to form. If not treated, this infection can spread to other parts of the body, such as the sinuses, jaw, or brain.
What happens if you have pulp necrosis?
Dental pulp necrosis leads to increased risk of: Dental abscesses (buildup of pus that forms inside the teeth or gums) Sinusitis (s inus infections ) Periodontal disease (gum disease) Skin irritation around the mouth. Bone loss in the jaw. Further tooth decay.
What causes pulp necrosis in teeth?
Dental pulp necrosis leads to increased risk of: 1 Dental abscesses (buildup of pus that forms inside the teeth or gums) 2 Sinusitis (sinus infections) 3 Periodontal disease (gum disease) 4 Skin irritation around the mouth 5 Bone loss in the jaw 6 Further tooth decay
What is the pulp chamber in a tooth?
Inside each tooth is a small space called the pulp chamber. This chamber has blood vessels and nerves embedded in tiny pieces of flesh— the “pulp” of the tooth.
What is the first step in a root canal?
The first step in a root canal is a pulpectomy. The dentist removes the damaged and infected pulp tissue. The pulp chamber is emptied and cleaned. The dentist might also apply some medicine to the pulp chamber to make sure no new bacteria can grow.
Can infection cause tooth pain?
While these are usually protected by the dentin and enamel of the tooth, infection and injury can still cause damage, killing some of the cells there. In the early stages of pulpitis, or infection of the pulp, a person might have extra sensitivity. For example, cold drinks and food might feel extra cold and painful.
Can a tooth be saved with a root canal?
The empty space is then filled in, and a crown is placed on the tooth to seal it. Extraction/Surgery. When a dead tooth can’t be saved with a root canal, a dentist may opt for extraction, removing it entirely. The tooth might then be replaced with a fixed implant or a dental bridge.
Can cold drinks cause tooth pain?
For example, cold drinks and food might feel extra cold and painful. There might also be feelings of pressure or dull, aching pain. By the time dental pulp necrosis sets in, the nerve endings in the pulp have died, and there is no longer any sensation in the tooth (including pain). However, often there will be discoloration of the tooth.
What is pulp necrosis?
Pulp necrosis is a clinical diagnostic category indicating the death of the pulp and nerves of the pulp chamber and root canal of a tooth which may be due to bacterial sequelae, trauma and chemical or mechanical irritation. It is often the end result of many cases of dental trauma, caries and irreversible pulpitis .
How to detect pulp necrosis?
Thermal testing is a common and traditional way used to detect pulp necrosis. These tests can exist in the form of a cold or hot test, which aims to stimulate nerves in the pulp by the flow of dentine liquid at changes in temperature. The liquid flow leads to movement of the odontoblast processes and mechanical stimulation of pulpal nerves.
Why does tooth avulsion cause pulp necrosis?
When a tooth is displaced from its normal position as a result of dental trauma, it can result in pulp necrosis due to the apical blood supply being compromised. This might be due to displacement of the tooth through avulsion or luxation. Furthermore, if the tooth is severely damaged, it could lead to inflammation of the apical periodontal ligament, and subsequently pulp necrosis.
How do odontoblasts decrease in size?
The odontoblast cell bodies decrease in number and size before any inflammatory changes occur. The outward flow of tubular fluid can cause the nuclei of odontoblasts to be aspirated into the dentinal tubules. The odontoblasts may also be permanently damaged which causes them to release tissue injury factors which can then influence adjacent odontoblasts and underlying connective tissue. Odontoblasts can undergo vacuolization, a decrease in the number and size of the endoplasmic reticulum, and degeneration of mitochondria. It is unknown by which process ( apoptosis or necrosis) the odontoblasts die.
Where is the pulp located in a tooth?
The dental pulp is located in the centre of a tooth, made up of living connective tissue and cells. It is surrounded by a rigid, hard and dense layer of dentine which limits the ability of the pulp to tolerate excessive build up of fluid.
What are the inflammatory mediators in the inflammatory response?
In response to bacterial assault and tissue injury non-specific inflammatory mediators are released. These inflammatory mediators include histamine, bra dykinin, serotonin, i nterleukins (IL) and metabolites of arachidonic acid. They can interact with neuropeptides ( substance P) and calcitonin gene-related peptide (CGRP) during the inflammatory response. Destruction of the nerve fibres causes neuropeptides to be released into pulp. The neuropeptides can cause an increase vascular permeability and vasodilation. The filtration of serum proteins and fluid from the vessel causes the tissue to become oedematous. The tissue pressure increases as the blood volume and interstitial fluid volume rises. The thin-walled venules are compressed and the resistance to flow in these vessels increases. This is accompanied with a decrease in blood flow causing an aggregation of red blood cells and subsequent increase in blood viscosity. This tissue also becomes ischaemic which suppresses the cellular metabolism in the area of the pulp that is affected. This causes necrosis. Necrosis is a histological term that means death of the pulp. It does not occur suddenly unless there has been trauma. The pulp may be partially necrotic for some time. The area of cell death enlarges until the entire pulp is necrotic. Bacteria invade the pulp which causes the root canal system to become infected. Teeth that have total pulpal necrosis are usually asymptomatic except for those that have inflammation which has progressed to the periradicular tissues.
Is internal root resorption a sign of pulpal necrosis?
Internal root resorption may be an indication of pulpal necrosis though it is not possible to diagnose accurately with radiographic presentation of this alone. This is because the pulp tissue apical to the resorptive lesion will still be vital to allow active resorption to take place, it provides the clastic cells with nutrients via a viable blood supply.
What is pulpectomy in primary teeth?
Pulpectomy in primary teeth. Pulpectomy is the complete removal of all pulpal tissue from the tooth. Pulpectomy can only be considered for primary teeth that have intact roots. Any evidence of root resorption is an indication for extraction.
What happens when a tooth avulsions?
The tooth is “separated” from the socket due mainly to tearing of the periodontal ligament that leaves viable periodontal ligament cells on most of the root surface. In addition, small and localized cemental damage occurs from the crushing of the tooth against the socket.
Why do teeth turn yellow?
Pulp necrosis can result from bacterial, mechanical, or chemical irritation of the pulp. These teeth require endodontic treatment prior to bleaching. Tooth trauma may result in tooth darkening due to internal bleeding from the pulp. The teeth may become gray or black-brown and then turn dark yellow-brown.
Can periradicular abscess be treated in one visit?
Patients who present with pulp necrosis with or without asymptomatic periapical pathosis (chronic apical periodontitis, chronic apical abs cess, condensing osteitis) may be treated in one visit , based on the best available information. When patients present with acute symptoms caused by pulp necrosis and acute periradicular abscess, obturation is generally delayed until the patient is asymptomatic. However, more than 20 years ago, investigators demonstrated that cases with soft-tissue swelling could be completed in one visit with appropriate endodontic treatment, incision for drainage, and a regimen of antibiotics.296 Management of these patients, however, may be more difficult should problems persist or become worse after the completion of treatment.
Can a pulp canal be obliterated?
A moderate injury typically caused pulp canal obliteration. And a severe injury often provoked pulp necrosis. There is usually no need for endodontic treatment in cases of mild injury because the pulp is likely to survive undisturbed.
Can you obturate a root canal?
Obturation of the root canal space in a primary tooth must not interfere with normal exfoliation of the permanent successor. This requires a resorbable paste root filling. The exception to this would be where it is planned to retain a primary tooth that does not have a permanent successor.
What is dental immaturity?
Dental immaturity is defined by the lack of apical closure. Necrotic immature permanent molars have a poor long-term prognosis and, except in exceptional circumstances, these teeth should be removed (see Extraction of first permanent molars, Chapter 14). However, retention of such teeth may be important for alveolar development, behavioural reasons or may facilitate subsequent orthodontic treatment by holding space until the optimal time for extraction.
What causes pulp necrosis in dogs?
Pulp necrosis may result from direct pulp exposure (e.g., complicated crown fractures), indirect pulp exposure (e.g., uncomplicated crown fractures, attrition, or abrasion), irreversible pulpitis in an otherwise intact tooth (e.g., gray–discolored, intact canine teeth), secondary to malformations, or as a result of severe periodontitis.15–19 The inevitable sequela of untreated pulp necrosis is inflammation in the tissues surrounding the apex, which can result in destruction of the periapical bone and soft tissues. 20 Therefore, teeth with necrotic pulp should be treated, either by endodontic therapy (root canal treatment) or extraction.
What is the best treatment for necrotic immature teeth?
A conventional method for treatment of necrotic immature teeth is the apexification, which aims to induce a calcified barrier to provide an apical stop for the root canal filling [ 13, 14]. Calcium hydroxide and mineral trioxide aggregate (MTA) are the most commonly used materials for apexification.
What causes periapical pathologies?
Dental caries, acute trauma, and dental anomalies can induce pulp necrosis and periapical pathologies. Importantly, root formation stops at the moment that the pulp undergoes necrosis, which results in teeth with open apices and thin root walls.
Can a nonvital tooth be a PC?
A nonvital tooth is a prerequisite to PC formation, though many nonvital teeth are initially asymptomatic. 25 In dogs, few necrotic and/or infected teeth are associated with clinical symptoms recognizable by pet owners. 33 The only evidence of pulp necrosis may be intrinsic tooth staining.33 In humans, most PC are asymptomatic and discovered during routine dental radiographic examinations as round to ovoid, well-circumscribed, unilocular periapical lucencies that are contiguous with the lamina dura of the involved tooth.14,25 Depending upon the stage at diagnosis, some cysts in dogs may demonstrate relatively wide areas of radioluceny ( Fig. 47.2A ). 4,5 Radiographically, a PC cannot be distinguished from a granuloma. 14,25 With longstanding PC, resorption of the affected tooth as well as adjacent teeth may occur ( Fig. 47.2B ). 4,14 With periapical granulomas, resorption of the affected tooth may be seen; however, resorption of adjacent teeth would be unexpected. 25 Although some types of ultrasound and computed tomography scans have demonstrated ability to differentiate between periapical granulomas and cysts, the gold standard for definitive identification of a periapical cyst versus a granuloma is histopathologic assessment through serial sections of lesions removed in their entirety. 25,31,34,35
What are the two types of insults that cause endodontic disease?
Two categories of insult that most commonly cause endodontic disease are bacterial infection and dental trauma. Dental pulp responds to injury in a manner similar to that of other connective tissues. However, the circulation is very limited and the tissue is confined within a rigid space that restricts its ability to swell. Trauma, inflammation, or infection of the pulp tissue can either heal or progress to irreversible pulpitis or pulp necrosis.
What happens if a tooth is subluxated?
In a subluxation, the periodontium has been damaged so that the tooth is loosened in its alveolus. Tooth mobility is limited to increased horizontal movement. The tooth has not been displaced in a vertical direction. No treatment is indicated except soft food and no toys for a week. Pulp vitality of the traumatized tooth does need to be monitored radiographically (radiograph at the time of diagnosis and then a check-up radiograph 6 months later), as pulp necrosis is the most common complication. If this happens, the tooth requires extraction or referral for endodontic treatment (pulpectomy and rootfilling).
Where is Dens evaginatus found?
Dens evaginatus is found in 1–4% of Asian populations and 15% of Alaskan Yupik, Inupiat, and North American Indian populations, occurring mainly in mandibular premolars [ 7–11 ]. Dens invaginatus has an overall prevalence of 1–10% and is observed primarily in maxillary lateral incisors [ 12 ]. Collectively, these studies demonstrate ...
How to diagnose pulpitis?
Diagnosis. A dentist can diagnose pulpitis from a person’s symptoms, an examination of the teeth, and possibly X-rays. In some cases, the dentist may perform other tests, such as: A sensitivity test: The dentist will check to see if cold or hot stimuli cause pain and discomfort.
What is the purpose of an electric pulp test?
These tests can help the dentist to determine the extent of the damage, and possibly save the pulp.
What causes tooth pain and swelling?
The dental pulp comprises soft connective tissue, nerves, and the blood supply for the tooth. Pulpitis causes pain, swelling, and sensitivity. A bacterial infection from a cavity is typically the cause. This article will look at what it is, as well as the symptoms, causes, diagnosis, and treatment options.
What is the term for inflammation of the pulp of the tooth?
Pulpitis is inflammation of the dental pulp. It is how a dentist might describe ‘toothache.’. The pulp inside a tooth consists of vascular tissues, blood supply, nerves, and connective tissue. When the pulp is inflamed, a person may experience pain from the tooth’s nerve. Pulpitis can be reversible or irreversible.
Can a dentist remove a tooth?
The dentist will typically perform a root canal treatment to remove the dying pulp. Alternatively, a dentist may remove the entire tooth, although this is not typically the first line of treatment if they can save the tooth. A dentist will not recommend systemic antibiotics as a treatment for irreversible pulpitis.
Can antibiotics help with pulpitis?
A dentist will not recommend systemic antibiotics as a treatment for irreversible pulpitis. This is because antibiotics will not alleviate the pain and heal the nerve inside the tooth.
What is pulpitis in teeth?
If left untreated, pulpitis can lead to a periapical abscess, otherwise known as a dental abscess, which is a localized infection in the bone or soft tissues. A person may notice a pocket of pus beside their tooth. Cellulitis may occur if the infection spreads to local tissue spaces and causes widespread swelling.
What is the diagnosis of pulpitis?
Diagnosis of Pulpitis. Diagnosis is based on the history and physical examination, which makes use of provoking stimuli (application of heat, cold, and/or percussion). Dentists may also use an electric pulp tester, which indicates whether the pulp is alive but not whether it is healthy.
What is the treatment for pulpitis?
Treatment of Pulpitis. Antibiotics (eg, amoxicillin or clindamycin) for infection that cannot be resolved with local measures. In reversible pulpitis, pulp vitality can be maintained if the tooth is treated, usually by caries removal, and then restored.
What is the term for inflammation of the pulp of the tooth?
Pulpitis. Pulpitis is inflammation of the dental pulp resulting from untreated caries, trauma, or multiple restorations. Its principal symptom is pain. Diagnosis is based on clinical findings, and results of x-rays and pulp vitality tests.
How long does it take for a tooth to stop hurting after a reversible pulpitis?
When the stimulus is removed, the pain ceases within 1 to 2 seconds.
What is Merck and Co?
Merck & Co., Inc., Kenilworth, NJ, USA is a global healthcare leader working to help the world be well. From developing new therapies that treat and prevent disease to helping people in need, we are committed to improving health and well-being around the world. The Merck Manual was first published in 1899 as a service to the community. The legacy of this great resource continues as the Merck Manual in the US and Canada and the MSD Manual outside of North America. Learn more about our commitment to Global Medical Knowledge.
When was the Merck Manual first published?
The Merck Manual was first published in 1899 as a service to the community. The legacy of this great resource continues as the Merck Manual in the US and Canada and the MSD Manual outside of North America. Learn more about our commitment to Global Medical Knowledge.
Is pulpitis reversible?
Sometimes infection develops (eg, periapical abscess, cellulitis, osteomyelitis). Pulpitis may be reversible or irreversible. In reversible pulpitis, the pulp is not necrotic, a cold or sweet stimulus causes pain that typically lasts 1 ...
What is the treatment for infected pulp?
Dental pulp that is infected is normally treated with a root canal procedure. The dentist may do it him or herself, or they may refer the patient to an endodontist. Endodontists specialize in root canals.
What is the pulp chamber?
July 28, 2020. By Staff. Deep inside the center of every tooth is an area called the pulp chamber. An infection in the pulp chamber can be painful and lead to serious dental issues.
What is the term for a tooth that is infected with bacteria?
An infection occurs when disease-causing bacteria invade living tissue. The pulp inside a tooth is living tissue too, and so can become infected. The condition is sometimes referred to as pulpitis . Typical indications of a dental pulp infection are toothache pain, especially while chewing, and sensitivity to hot or cold food and drink.
What is the first step in a root canal?
Endodontists specialize in root canals. The first step is a pulpectomy, where the infected pulp tissue is removed from inside the tooth. The empty pulp chamber is cleaned and then filled. The final step is sealing the tooth so that no further bacteria can get inside.
What to do if you have an abscess in your tooth?
Extracting the tooth is often the only option. The lump that results from an abscess is filled with infected fluid. The dentist or endodontist first step will be to drain it. Antibiotics may be prescribed to stop the infection from spreading any further.
What is the pulp of a tooth made of?
The pulp is made up of nerves and blood vessels, surrounded by a protective layer called the dentin. Encasing the dentin is the hard, outer shell of the tooth: the enamel. Dentin is softer than enamel. If anything makes its way through the enamel to the dentin, the pulp inside the pulp chamber underneath is at risk of infection and decay.
What causes cavities in teeth?
Tooth decay is the result of acids and bacteria building up on teeth in the form of a sticky substance called plaque. If plaque isn’t cleaned off regularly, cavities can appear . Cavities start out as small holes in the tooth’s enamel, but can grow if they aren’t filled by a dentist.
Popular Posts:
- 1. "how to watch television" course review
- 2. which of the following is always illegal in the united states course hero
- 3. what is the difference between withdrawing and withholding life-sustaining treatment course hero
- 4. how long is a six month course of xeloda
- 5. how to schedule your 5 hour course with the ymca rome ny
- 6. consider the graph. what does it represent? ice cream utility course hero
- 7. what makes interpersonal communication a complex process?course hero
- 8. how many course were at el bulli
- 9. which acc campus has the 2359 wind course
- 10. how much is an ap course weighted